Colonoscopy
What is a colonoscopy?
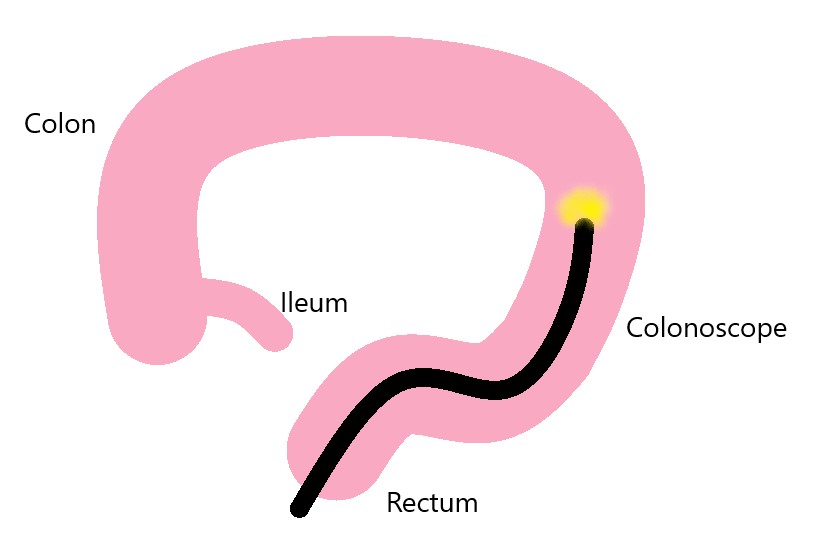
Colonoscopy is an examination of the colon, rectum and sometimes, the last portion of the small intestine (ileum) using a flexible telescope called a colonoscope.
During the examination, a number of small procedures can also be carried out, including:
- Taking a small tissue sample (biopsy)
- Removal of polyps – a growth on the surface layer of colon or rectum. Some polyps may become bowel cancer and can be removed by your gastroenterologist when detected
Why am I having a colonoscopy?
A colonoscopy can be used to look for bowel cancer or polyps, which are growths on the lining of the colon that can sometimes be cancerous or may grow to be cancerous. A colonoscopy may be performed to find the cause of signs and symptoms including:
bleeding from the rectum
- blood in the stools
- pus or mucous in the stools
- unexplained abdominal pain
- changes in bowel habits such as unexplained and long-lasting diarrhoea
- screening and surveillance for colorectal cancer
Risks of a colonoscopy
Colonoscopy is a safe procedure, although complications may rarely occur. Complications such as perforation (puncture) of your bowel wall or major bleeding (e.g. requiring blood transfusion) are very uncommon and occur in less than 1 in 1,000 procedures.
When other procedures or operations are carried out through the colonoscope the risk may be greater and this will depend on the condition being treated. Ask your gastroenterologist performing the colonoscopy, about the risks related to any additional procedures or operations.
Colonoscopy usually involves anaesthetic sedation. Risks of sedation are uncommon but may include difficulty breathing and abnormal heart rhythms.
Preparation
Tell your doctor before the procedure if you:
- are sensitive (allergic) to any drug or substance
- are taking blood thinning medications
- have heart valve disease
- have a pacemaker or defibrillator
You will be required to undergo bowel preparation to clean your bowel so that your colon surface can be adequately examined. Please carefully follow the instructions provided to you as complete bowel cleansing is essential to ensure best results from the examination.
Please click here to view bowel preparation instructions.
What happens during a colonoscopy?
You will be given an intravenous sedative before the procedure. The medications provide deep sedation so that you will generally not have any recollection of the procedure or feel pain. You will lie on your left-hand side and colonoscope is gently inserted through your bottom and up into the colon. Gas is introduced to help the colonoscope pass.
Once the colonoscope has reached the end (caecum or ileum), your gastroenterologist will slowly withdraws it while looking carefully at the colon’s surface. Photographs may be taken. If polyps are found, they are removed and the tissue is sent for analysis. Polyp removal or biopsy may cause bleeding but is usually self-resolving. Rarely bleeding can occur up to 2 weeks after polyp removal.
After a colonoscopy
After the colonoscopy, it is possible that you may experience abdominal bloating or mild cramping. These symptoms usually subside within 1 hour. You may be offered a drink and something light to eat after you are awake. Usually you can go home after about four hours.
For your personal safety following the sedated procedure, we require that a friend or relative to escort you from our day ward to take you home. A responsible adult should also stay with you overnight after your procedure.
After the sedative you should not:
- drive a car or operate machinery for 24 hours
- sign any legal documents until the next day
- undertake any other activities likely to place you at risk
If you require help
Please:
- Call our practice during working hours (9am – 5pm, Monday to Friday)
- Speak with your GP
- Call Health Direct
- Attend your nearest emergency department or call 000
