Gastroscopy
What is a gastroscopy?
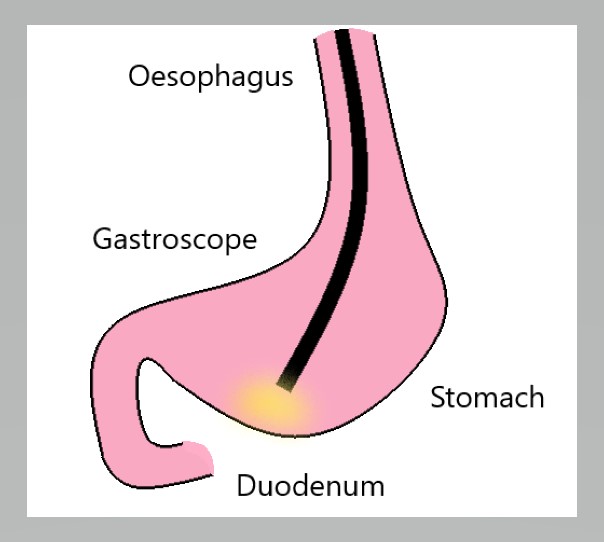
Gastroscopy (or endoscopy) is an examination of the oesophagus (food pipe), stomach and duodenum (first part of the small bowel) using a flexible telescope called a gastroscope.
During the examination, a number of small procedures can also be carried out, including:
- taking a small tissue sample (biopsy)
- stopping bleeding from an ulcer
- removal of polyps
Why am I having a gastroscopy?
Patients have gastroscopy for several reasons. For example, there may be symptoms such as indigestion, abdominal discomfort or bleeding suggesting an ulcer. Alternatively, the procedure may be done to treat certain conditions.
Risks of a gastroscopy
Complications of a gastroscopy, such as perforation (puncture) of your stomach or duodenal wall or major bleeding (for example, requiring blood transfusion) are extremely uncommon. When the examination involves only inspection of the bowel or taking a biopsy, these complications occur in less than 1 in 10,000 procedures.
When other procedures or operations are carried out through the gastroscope the risk may be greater and this will depend on the condition being treated and the operation proposed. Ask your gastroenterologist performing the gastroscopy, about the risks related to any additional procedures or operations.
Very uncommonly, there may be damage to teeth from the mouthguard used during the gastroscopy. If you have false or loose teeth, please inform the staff before the test.
Gastroscopy usually involves anaesthetic sedation. Risks of sedation are uncommon but may include difficulty breathing and abnormal heart rhythms.
Serious sedation reactions may be more common in patients with severe heart or chest disease. These complications are usually avoided by administering oxygen during the procedure and monitoring the oxygen level in the blood. Some patients wish to have the gastroscopy without sedation, so if this applies to you please discuss this when you attend for the examination.
Preparation
You will usually be asked not to eat or drink for 6 hours before gastroscopy. Tell your doctor before the procedure if you:
- are sensitive (allergic) to any drug or substance
- are taking blood thinning medications
- have heart valve disease
- have a pacemaker or defibrillator
On the day of the procedure
Wear something comfortable and loose with short sleeves. If you are an outpatient, report to the hospital as outlined in your appointment letter.
What happens during a gastroscopy?
A spray may be applied to the throat to numb it, and it is important that any dentures or plates are removed. You will be given a sedative injection through a vein in your arm before the procedure. Your doctors will then gently insert the gastroscope through your mouth and into the oesophagus, stomach and duodenum. Any discomfort at the back of the throat is minimised by using the throat spray and sedative injection, and is helped by calm deep gentle breathing during the test.
After a gastroscopy
Any sedative you are given before the procedure is very effective in reducing discomfort. However, it may also affect your memory for a few hours afterwards. Even when the sedative appears to have worn off, you may be unable to recall details of your discussion with your gastroenterologist or nursing staff. For this reason a relative or friend should come with you if possible.
For your personal safety following the sedated procedure, we require that a friend or relative to escort you from our day ward to take you home. A responsible adult should also stay with you overnight after your procedure. Following the procedure you may have a slightly sore throat for up to 24 hours.
After the sedative you should not:
- drive a car or operate machinery for 24 hours
- sign any legal documents until the next day
- undertake any other activities likely to place you at risk
If you require help
Please:
- Call our practice during working hours (9am – 5pm, Monday to Friday)
- Speak with your GP
- Call Health Direct
- Attend your nearest emergency department or call 000
